Meet the Team
Expert Care, Personal Attention — From the Team That Moves You Forward
Bluegrass Orthopaedics features an exceptional team of fellowship-trained physicians, physician assistants, and physical therapists who specialize in all areas of musculoskeletal health — from sports medicine, hand & wrist, and foot & ankle to spine, shoulder, hip, and knee care. Use the filters below to find the right provider by specialty, location, or care type, and connect with a provider dedicated to restoring your movement and quality of life.
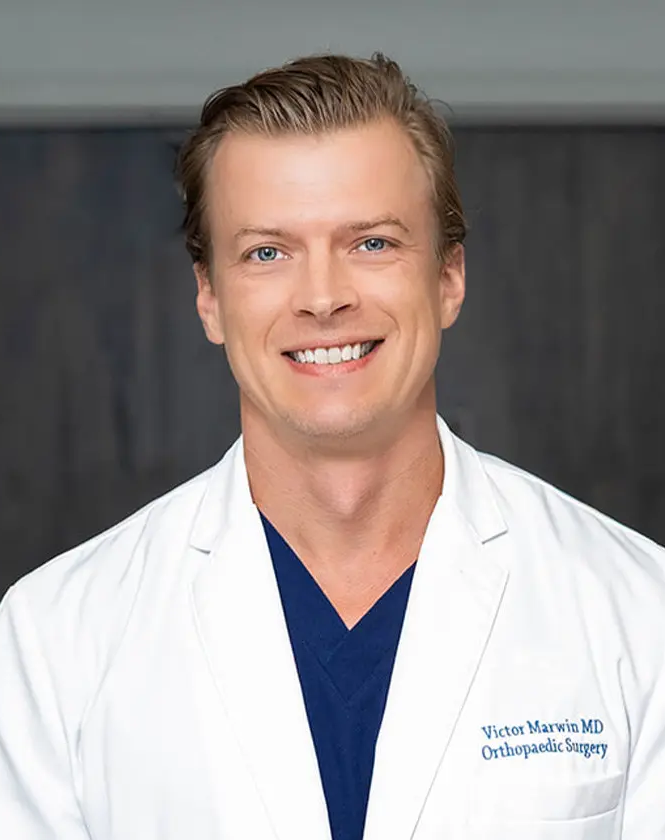
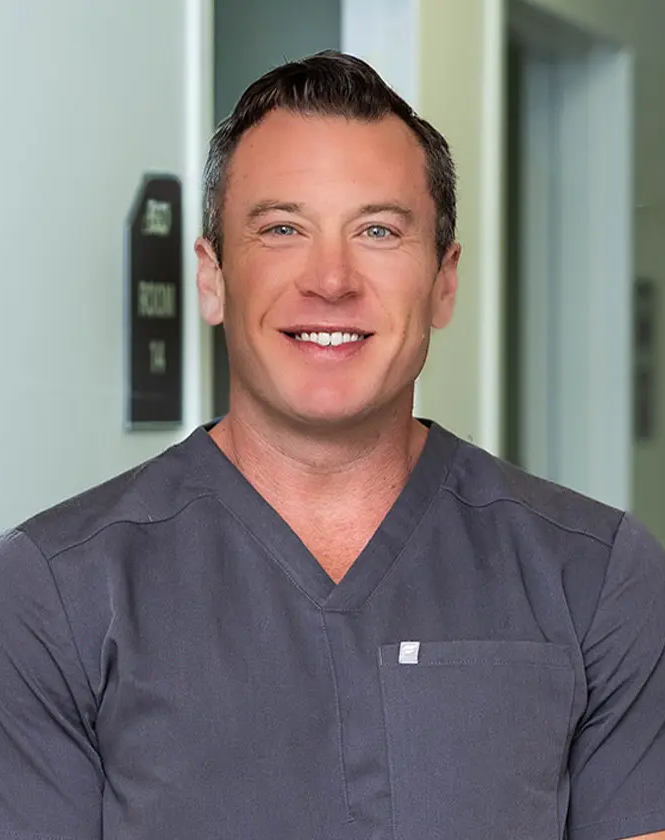
Physicians
Charles "Ched" Crouse, MD
General Orthopedics, Joint Replacement, Sports Medicine, Hip & Knee
View BioPhysician Assistants & Nurse Practitioners
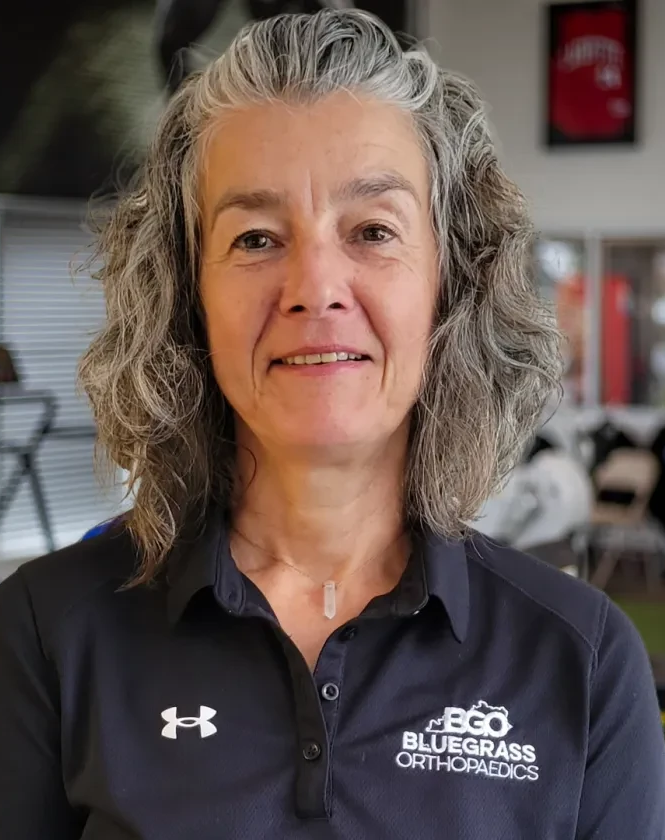
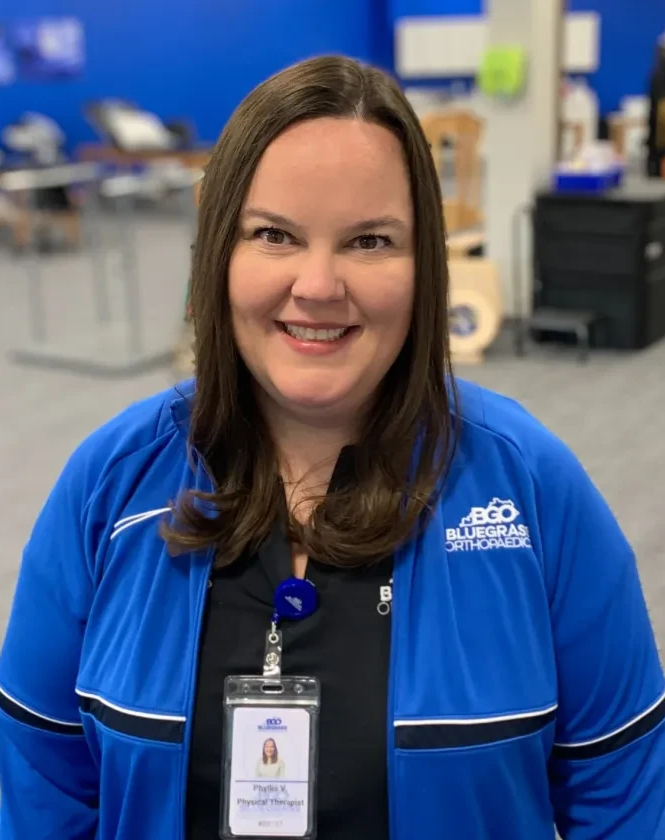
Physical & Occupational Therapists

David Escobar, MS, PT, Cert DN, Cert SMT, Dip Osteopractic, FAAOMPT, Cert MSKUS
Richmond Clinic Director
View BioAthletic Trainers

Katelin Estes, MSAT, ATC
View Bio
Mandy Flaig, DAT, ATC
View Bio
Sammy Fluck, MSAT, ATC
View Bio
Bailey Reecer, MSAT, ATC
View Bio
Collin Schneider, MSAT, ATC
View Bio